Hepatitis C
- Hepatitis C is a liver disease caused by hepatitis C virus (HCV) infection.
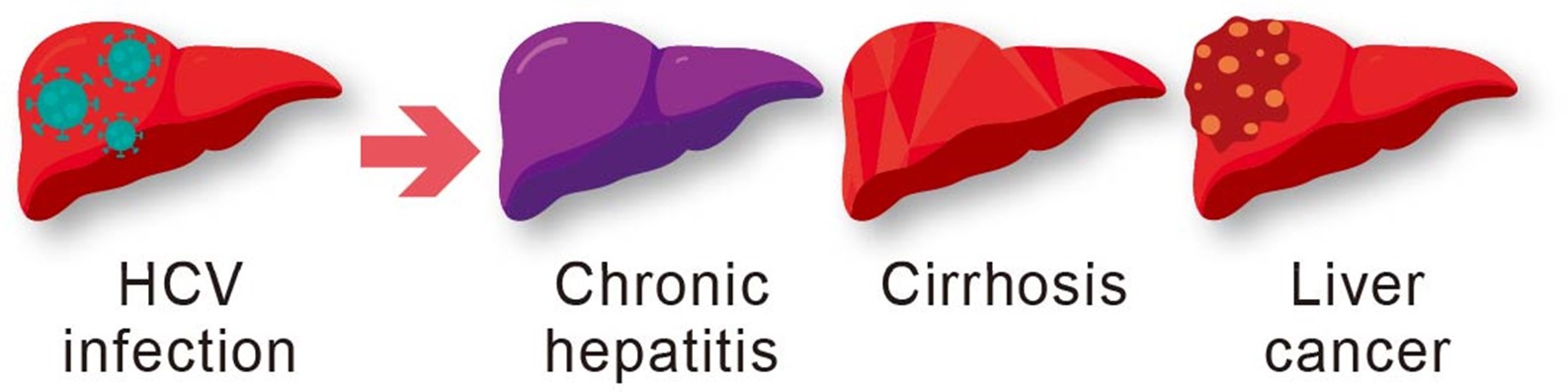
- Around 70% of people infected with HCV will develop chronic hepatitis (HCV can still be detected 6 months after acute infection), which may lead to cirrhosis and liver cancer.
- The incubation period is around 6 to 9 weeks (ranges from 2 weeks to 6 months).
- Newly acquired HCV infection is mostly asymptomatic. Some people with acute HCV infection may exhibit symptoms indistinguishable from hepatitis of other causes, such as fever, fatigue, loss of appetite, nausea, vomiting, upper abdominal discomfort, tea-coloured urine and jaundice (yellowing of skin and the whites of eyes).
- Hepatitis C can remain asymptomatic until decades after infection, when signs and symptoms develop secondary to serious liver damage.
Epidemiology in Hong Kong
- WHO estimates that 0.8% of world population is chronically infected with HCV in 2019.
- Some specific populations are at higher risk of HCV infection, such as people who inject drugs, recipients of potentially contaminated blood products, HIV-positive people, people who have had tattoos or piercings with inadequately sterilised instruments and men who have sex with men.
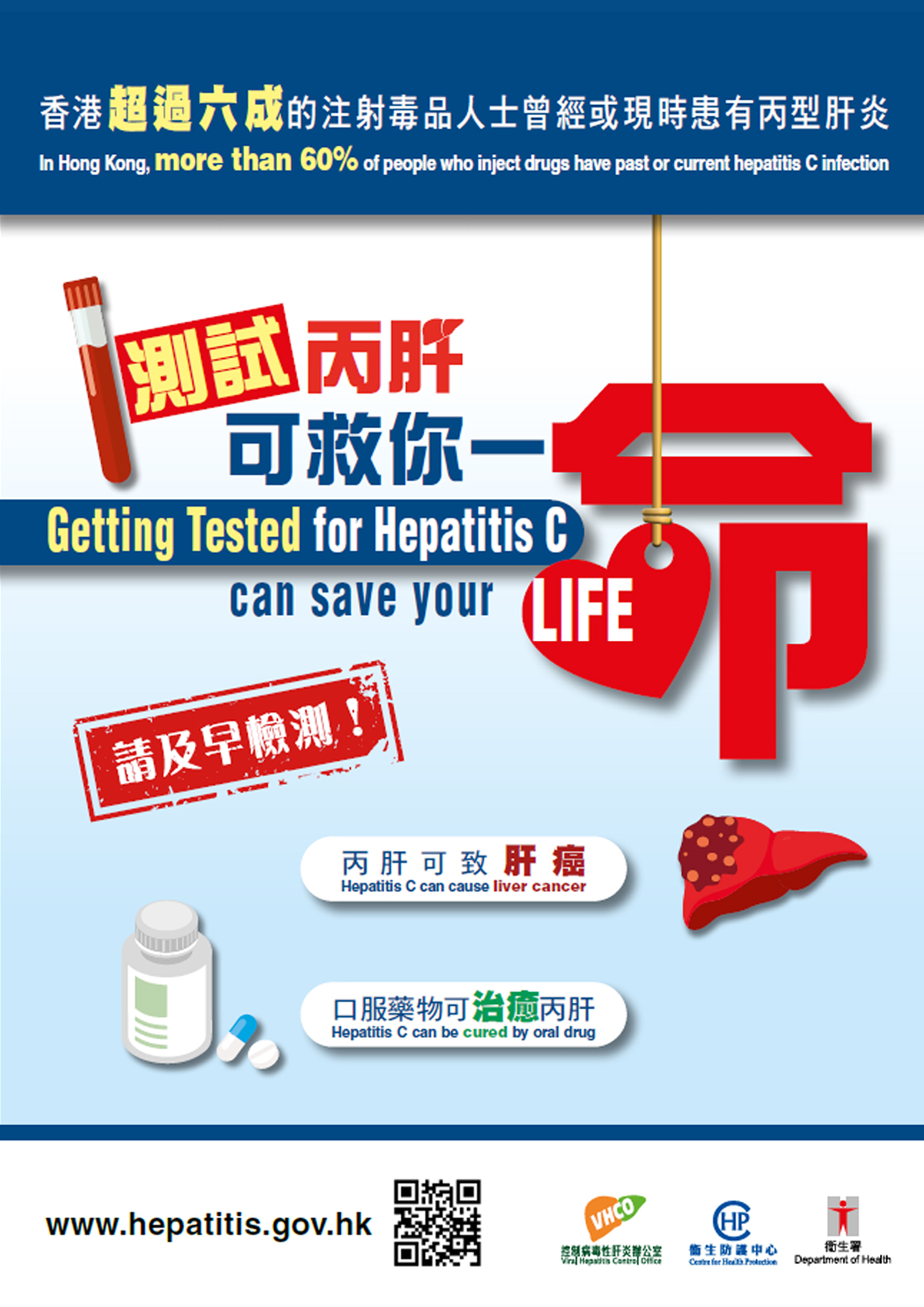
- An estimated 0.3% of Hong Kong population have ever been infected with HCV, but prevalence of HCV infection is higher among people who inject drug (more than 60% have past or current hepatitis C infection).
- As derived from the results of Population Health Survey (PHS) 2020-22, about 17 000 people have hepatitis C in Hong Kong.
- Please click here for the Thematic Report on Viral Hepatitis (PHS 2020-22).
Transmission of hepatitis C
- HCV is most commonly transmitted through contact with blood, for example
- sharing needles, syringes or other equipment for injecting drugs among people who inject drugs
- reusing inadequately sterilised medical equipment
- transfusion of unscreened blood and blood products
- occupational exposure to blood or body fluid with HCV in healthcare setting
- Sexual transmission of HCV is uncommon. However, it can occur if both partners have skin or mucosal lesions and do not use condoms during sex, especially during sexual practices that lead to exposure to blood. The risk of sexual transmission of HCV increases among men who have sex with men, HIV-positive people and those who have sexually transmitted infection.
- Vertical transmission from an infected mother to her baby during labour ; estimated risk of mother-to-child transmission is about 4 - 8%.
- HCV is not transmitted through social contact, such as sharing eating utensils, dining together, hugging, holding hands and kissing.
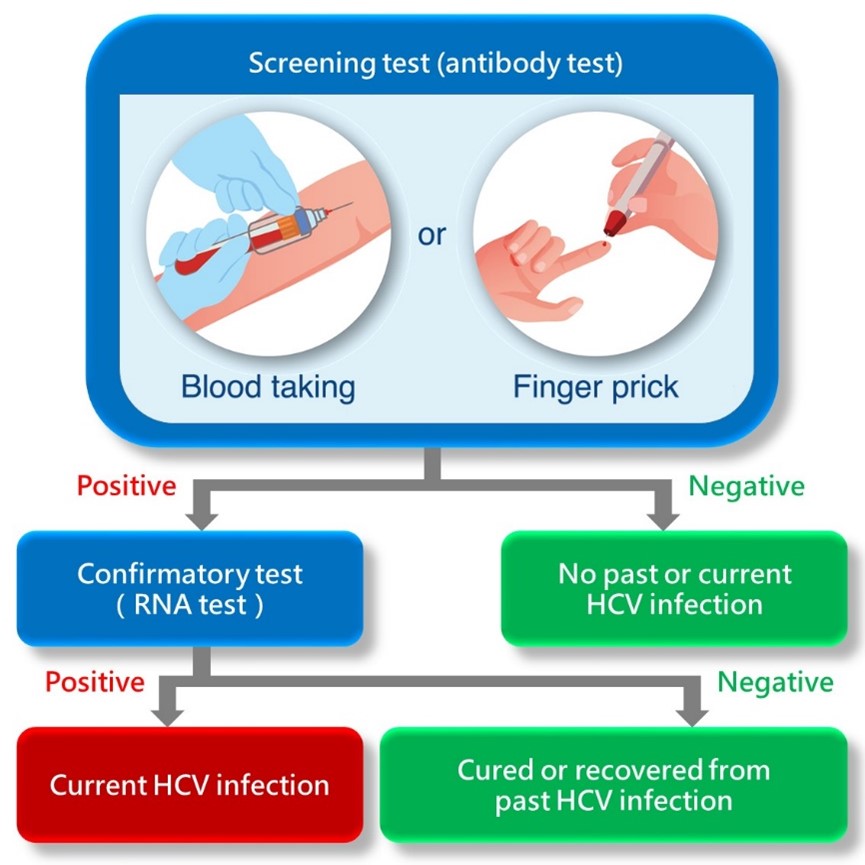
Blood Test is required to diagnose hepatitis C
Screening test: Antibody against HCV (Anti-HCV)
- A positive result indicates HCV infection at some point in one’s life, and it should be followed by a confirmatory test.
- Anti-HCV is produced following infection with HCV, but it does not confer immunity to HCV infection.
Confirmatory test: HCV ribonucleic acid (HCV RNA)
- A positive result confirms a current HCV infection.
- A negative result indicates cure or recovery from past HCV infection.
People tested positive for both anti-HCV and HCV RNA are diagnosed as having HCV infection, and should be treated.
Treatment of hepatitis C
- Currently, direct-acting antivirals (DAA) are first-line drugs of hepatitis C treatment.
- Highly effective (over 95% of HCV infection can be cured)
- Oral administration (do not require injection)
- Treatment usually takes around 8 - 12 weeks
- Minor side effects
- As compared with traditional treatment using PEGylated interferon and ribavirin, DAA are not only better tolerated, but also more effective.
- With successful clearance of HCV, the risk of progression to cirrhosis and liver cancer and dying from liver diseases can be significantly reduced. However, regular examination is still required if there is deteriorated liver function, cirrhosis or its complication before treatment.
- As treatment does not confer protective immunity, recovered hepatitis C patients should stop high-risk behaviours to prevent HCV re-infection.
Sustained virological response (SVR) is an indicator of treatment success.
A sustained virological response occurs when the blood test shows no detectable RNA in 12 weeks after treatment. People having achieved SVR after treatment are considered as cured, and will not transmit the virus to others.
Prevention of hepatitis C
There is no vaccine available against hepatitis C. The following measures should be taken to prevent hepatitis C:
- People who inject drug should stop injecting drugs and get into methadone treatment programme. Never share needles, syringes or other equipment that is potentially contaminated with blood
- Avoid sharing personal care items (e.g. razors and toothbrushes) that are potentially contaminated with blood
- Use condoms correctly and every time when you have sex
- Healthcare workers should always practise standard precautions, including handling and disposing needles and sharps properly and safely
- HCV infected persons should not donate blood, organs or tissue
Health education materials
- “Hepatitis C can cause liver cancer. Get tested and treated early” video
- "What You Need to Know About Hepatitis C" pamphlet
- “Getting tested for hepatitis C can save your life” pamphlet
- “Getting tested for hepatitis C can save your life” poster
- Presentation slides – Hepatitis C virus infection (only Chinese version available)